THE INESCAPABLE TRUTH

How seventeen people a day will suffer as they die

Warning
This report contains detailed and graphic accounts of physical and emotional distress that people have experienced at the end of life.

The experiences shared in this report are as harrowing as anything I have encountered as a Member of Parliament. I have had two bouts of cancer and am no stranger to the nastiness of the disease and its treatments, but nothing prepared me for the horror of what is described here.
In 2019 British people are being forced to endure unbelievable suffering at the end of life. Some will retch at the stench of their own body rotting. Some will vomit their own faeces. Some will suffocate, slowly, inexorably, over several days, their last moments of life disfigured by terror. Any one of us might suffer such a fate.
17 people died in this manner yesterday. 17 more will die that way today, and tomorrow.
This will continue to happen despite the best efforts of our wonderful hospices. It will continue to happen despite the care and compassion of palliative care nurses and doctors. It will continue to happen because the law refuses people in this position the right to relieve their suffering should that be their wish.
Those who oppose a change in the law point to the fact that palliative care works for the vast majority of people approaching the end of life. That is no consolation to the people for whom it does not. It is shocking to think Parliament could ever be content with a policy that has such disastrous consequences for so many people.
Of course assisted dying should be a last resort. Of course it should be tightly regulated and operate under strict safeguards, as it has done in many places around the world since the end of the last century. To still deny it altogether to dying people in the UK who cannot be helped by palliative care, to force them to undergo unbearable physical and psychological trauma instead, is a moral outrage.
If you are in doubt about the need for an assisted dying law I urge you to read this report and when you’ve reached the end ask yourself this:
What right do you have to refuse someone with a terminal illness, who has the mental capacity to make a choice, the means to avoid an agonising death?
Nick Boles MP

THE LIMITS OF PALLIATIVE CARE


At the end of life, some dying people experience severe pain and other symptoms that result in suffering.
Crucially, this suffering occurs even when high-quality specialist palliative care is present, meaning improving the provision of care will not address this problem. Specialists in palliative care and pain management whose interviews are featured in this report confirmed that they see cases where a person’s suffering cannot be relieved despite their best efforts.
In research commissioned for this report, the Office of Health Economics concludes that, even if every dying person who needed it had access to the excellent level of care currently provided in hospices, 6,394 people a year would still have no effective relief of their pain in the final three months of their life. This equates to 17 people dying in pain every day. Evidence suggests that if people suffering from other unrelieved symptoms during the dying process were included this number would be much higher.
PAIN
Pain can be severe at the end of life, as terminal illnesses can disrupt the body’s usual functions. Macmillan Cancer Support suggests around half of people who have cancer will experience some pain, though others have estimated the figure to be much higher.
The only thing in her life was pain. It was strong enough to bring her bubbling up from this cocktail of drugs she was being given.
Pain can be relieved through simple painkillers such as paracetamol and ibuprofen or opioids such as codeine, morphine and fentanyl. Other drugs such as antidepressants, steroids and psychoactive substances can also be involved in treatment. Non-pharmacological treatments such as talking therapies have been shown to successfully contribute to the management of pain.

Studies have shown that having pain controlled is the primary factor associated with having a good death. The BMA’s research into public and professional perceptions of end-of-life care found that being in pain at the end of life was a fear of both the public and doctors. Doctors viewed pain as something that could be managed, but acknowledged that it could not be eliminated entirely.
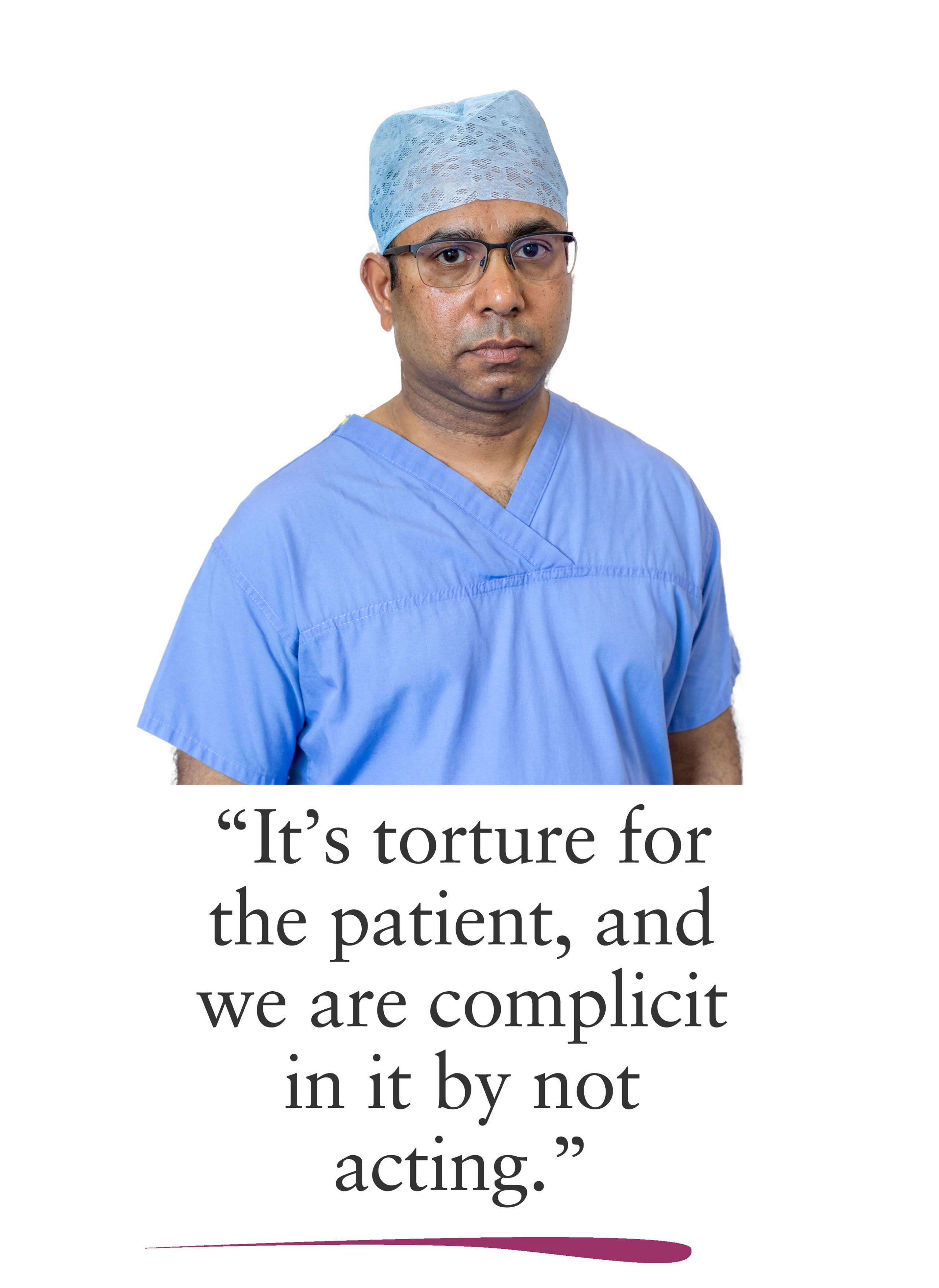
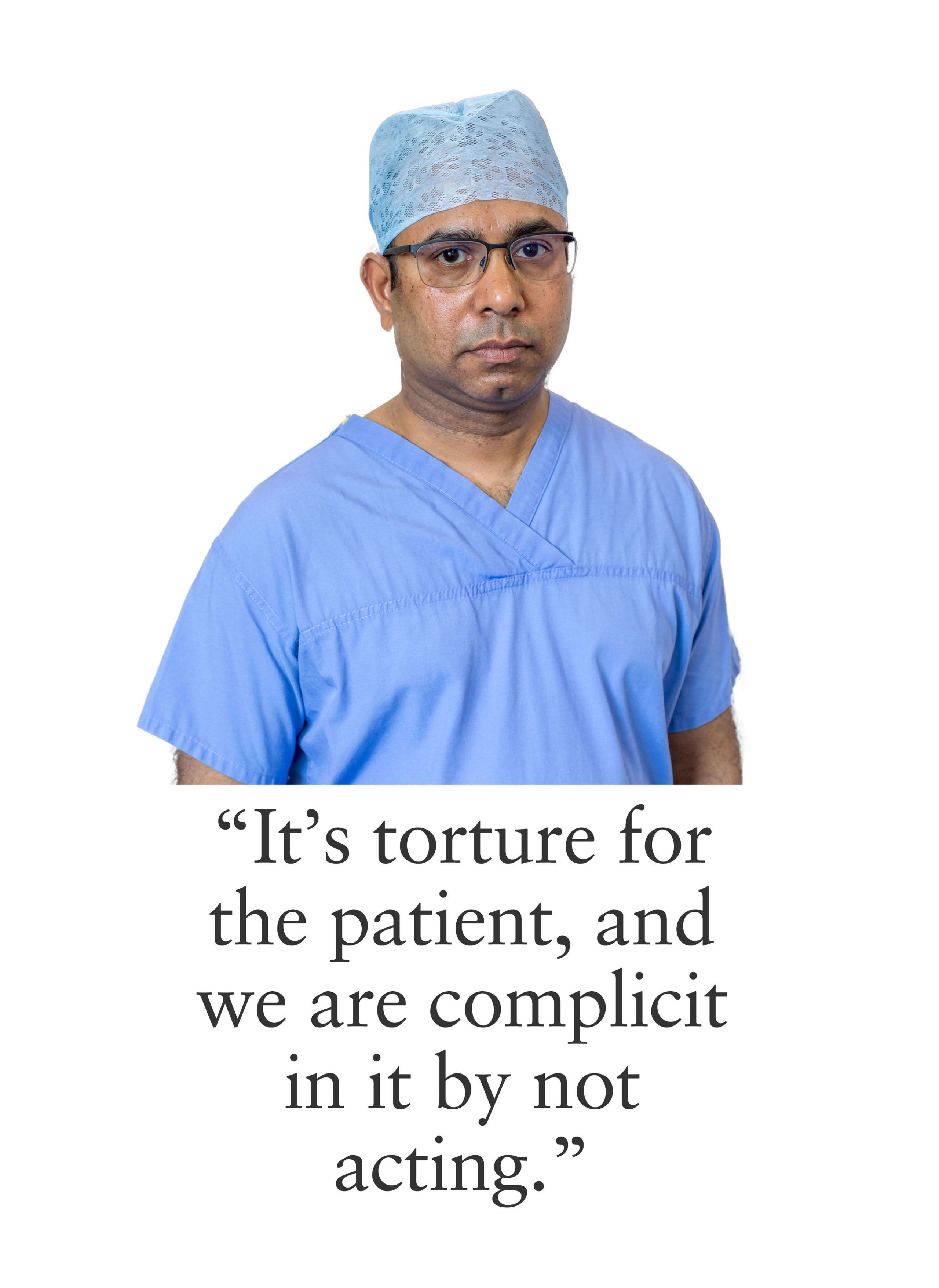
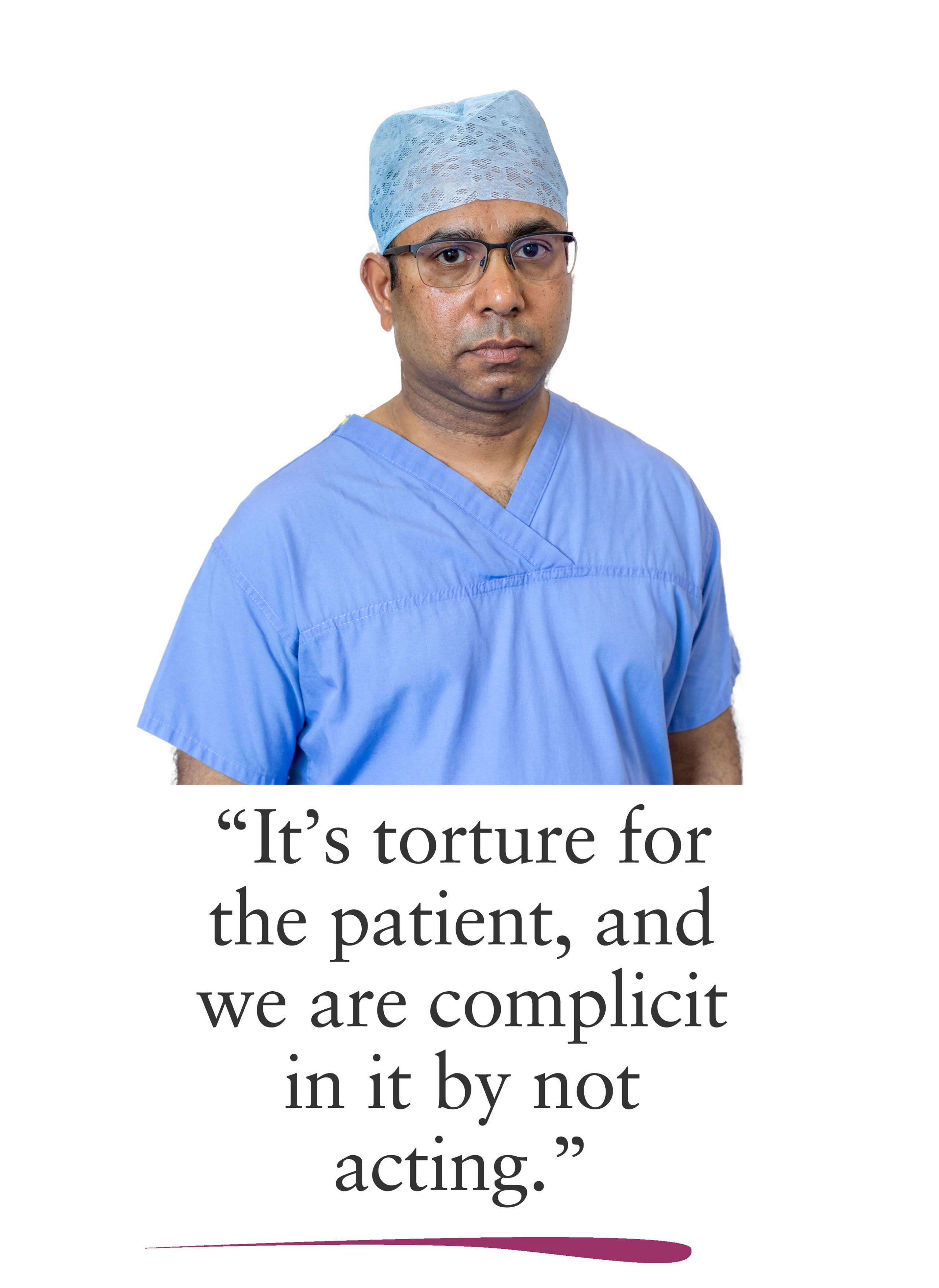
In the interviews featured throughout this report, healthcare professionals echoed this view.

I remember a patient from a couple of years ago who had very, very severe pain from a cancer that was affecting nerves in his back. He was in exceptionally difficult pain. He was young, he was married and they had a child. We tried lots of different medications and it was just getting us nowhere. We had gone through all the normal sedation routes and it was just not working.
Palliative care consultant
Dying people described the experience of living with pain and how it made them consider the level of pain they might suffer in the future and whether or not they would find it tolerable.
I know what pain is. Pain is where you cannot think about anything else, you're just rocking there thinking, 'Where's a gun? I want to go now.' I've had pain and if it was the case that it couldn't be controlled I would want to die. I don't want a life that has that amount of pain, to lose my identity. If I became somebody enveloped by pain, then at that point I don't want life.
Bereaved relatives described witnessing their loved ones in pain, even when they had access to specialist palliative care.
She was very positive, she was very stoic. She had palliative care in the house but then at the end of September she developed gangrene in one of her hands, which they said was due to the cancer and vascular problems. She was in excruciating pain.
One relative said her sister was not aware of how much pain she would be in at the end of her life. She was in a hospice and the palliative care team had told her they would ensure she had a peaceful death.
They did tell her that they would manage her pain. They kept saying that she wouldn’t be in pain. She was in pain. She was crying and sometimes she was yelping like a dog.
Complications of pain management
Approximately 10% of people have a genetic variation which can lead to complications in how they respond to pain relief medication. This genetic variation can mean pain relief is ineffective or that higher doses are required. Prolonged use of pain relief can also lead to the requirement for higher doses.
High doses of pain relief are associated with symptoms such as drowsiness, hallucinations, nausea, vomiting. Constipation is a common and difficult to manage side-effect of pain treatment and this will be explored in more depth below. These symptoms are shown to reduce quality of life and are often considered intolerable by patients.
Two of the problems all the way through were that she was allergic to anti-sickness and anti-pain medication. We tried everything. She was pacing all night, every night, and that was right through to the end.
Many interviewees, including professionals, bereaved relatives and dying people, highlighted the unpleasant side-effects that can result from pain relief medications. As well as physical symptoms, this included the difficult compromise people often have to make in order to preserve their mental clarity, at the cost of sacrificing relief of their pain.
National guidance on using strong opioids for pain relief recommends that professionals seek to find a dosage of pain relief where ‘a good balance exists between acceptable pain control and side-effects.’
Some of the painkillers I’m on have made me not quite as sharp mentally as I used to be. I’m still writing, I write plays and novels, and the idea of losing that creative part of myself is just unbearable.





UNCONTROLLABLE SYMPTOMS
Nausea and vomiting
Nausea and vomiting are common symptoms of terminal illnesses. Studies suggest around 50% to 60% of people with advanced cancer suffer from nausea and/or vomiting, with people under 65 and women more likely to be affected.
Nausea and vomiting are also common side-effects of pain relief treatment. Approximately one third of people who are given opioids experience nausea, though this side-effect has been shown to diminish over time. In one study, 22% of patients withdrew from opioids because of the severity of side-effects including nausea. Nausea and vomiting can be treated with antiemetics, but, as one study in a hospice found, even when guidelines are followed symptoms can persist in some people.

I think pain is not necessarily the worst symptom you can have. I think nausea is often worse and is often much harder to deal with. A lady I’m treating has nausea and we’ve been through the medication that we would use for nausea and it is not helping.
Palliative care consultant
Bowel-related symptoms
Constipation can be associated with abdominal and rectal pain, abdominal distension, anorexia, nausea and vomiting, urinary retention, and confusion. In 2008, a pan-European working group of palliative care professionals stated that constipation ‘is one of the most common problems in patients receiving palliative care and can cause extreme suffering and discomfort.’ The working group recognised that constipation can significantly reduce quality of life and has been found to rival or exceed pain in terms of the severity of distress it causes to dying people.
Similar to nausea and vomiting, constipation is a common side-effect of pain relief treatment. A review of existing evidence observed that constipation ‘occurs in almost every patient taking opioids and does not lessen with continued use.
The treatments available for constipation include laxatives, suppositories and enemas and these are widely regarded as effective. However, there is a consensus that more research on the treatment of constipation is needed.
Treatment can result in diarrhoea, incontinence and the need for rectal care, all of which can have a negative impact on a dying person’s sense of dignity. Therefore, the benefits of treatment have to be balanced against its side-effects.
She had bowel cancer and she basically wanted to be at home so she could just die looking out on her shed and garden with the family around her.
But she had to go into a hospice because of her toilet needs. Her bowel was blocked so she couldn’t pass anything. She’d had trouble passing for a few weeks at home.
Faecal incontinence is a common symptom of some cancers towards the end of life. It is also a side-effect of treatment for cancers in the abdominal area. One study found nearly half of patients receiving treatment for rectal cancer went on to suffer from incontinence. These side-effects have been shown to harm people’s physical, psychological, social, and emotional well-being. However, this does not always lead to an overall reduction in quality of life.
In 2014, clinical ethicist Ann Munro told The Guardian that there are symptoms of dying that doctors can do little to alleviate. One woman in her care was passing faeces through her vagina: ‘She said to me, “I don’t want to be here anymore. I want this to stop. What can you do about it?” She found it humiliating and grim and she was going to die.’
Passing faeces through the vagina occurs when a person has a rectovaginal fistula. The most common cause of these fistulas is childbirth, but they can occur as a result of cancers and radiotherapy treatment.
Munro also said ovarian and bowel cancers can often lead to people vomiting their faeces. Scottish palliative care guidelines acknowledge faecal vomiting as a potential symptom of bowel obstruction.

I have seen people who have got vomiting towards the end of life because they have partial bowel obstruction. They are able to take some sips of water. They are able to take a cup of tea, but an hour later it comes back accompanied by faeces. They are actually vomiting up their faeces.
Palliative care consultant
As part of a public conversation about legalising assisted dying in Australia, Angelique Flowers contacted the then Prime Minister Kevin Rudd to ask why he could not change the law to allow her a ‘peaceful death.’ Angelique was 30 when she was diagnosed with colon cancer and given just months to live. Following her death, her brother Damian said that in the last hour of her life ‘he held a bowl under his sister’s chin as she vomited faecal matter'.
Terminal haemorrhages
Terminal haemorrhages, also known as catastrophic haemorrhages, are a symptom of some cancers, most commonly in the head and neck, where tumours erode major blood vessels resulting in extensive and rapid blood loss that leads to death.
Terminal haemorrhages have been described as ‘rare but devastating’ events, primarily because treatment options are limited. When a terminal haemorrhage occurs, sedatives are administered in an effort to reduce distress for the dying person. But research suggests that this practice is largely ineffective because the person is likely to die before the effect of the sedative is felt. It has been proposed that the primary benefit of sedation in these circumstances may be the reassurance it offers to dying people who are at risk of a terminal haemorrhage, even if the palliative care team has doubts over the benefits sedation would offer should a haemorrhage occur.
Guidance for the management of terminal haemorrhages suggests more practical measures to reduce distress for dying people, as well as loved ones and healthcare professionals who are present, such as the use of dark sheets and towels to camouflage the extent of the blood loss. The reported incidence of terminal haemorrhages in patients with advanced cancer is between 3% and 12%. However, the evidence base for these estimates is unreliable, focussing on small-scale studies and expert opinion.

We’ve had people who have bled out suddenly, and you whack them with midazolam and you hope that they don’t know what’s going on. But then they pass away, so you can’t ever ask them.
Palliative care nurse
Malignant fungating wounds
Malignant fungating wounds develop when cancer breaks through the skin. These wounds occur more frequently in breast, head and neck cancers, but can occur in other circumstances. Symptoms include an unpleasant smell, pain, bleeding, itching and leakage. Fungating wounds can sometimes be treated with radiotherapy and chemotherapy, but it is unlikely that they will ever completely heal.

One lady had tumours in her abdomen, which were starting to eat their way out of her, actually coming out of her abdomen. The smell was horrific. It was basically dying flesh and she was still with us and her family’s memory of her was her decomposing while she was still alive. And there was nothing we could do to stop it. She went on for about a week and a half like this, literally decomposing from the inside out. She was unconscious and you just have to hope that she wasn’t aware of too much. You just wanted to do something, even if it was just getting rid of the smell for the family, but you couldn’t because it was everywhere.
Palliative care nurse
The prevalence of malignant fungating wounds is unclear. A survey in the UK in 1992 reported 2,417 new cases per year, with 5% of those cases caused by a primary tumour and 10% caused by metastatic disease. More recent research estimates that between 5% and 10% of patients with cancer develop a malignant fungating wound, although the true number may be higher as some patients do not present symptoms due to embarrassment. In one study, nine people with malignant fungating wounds resulting from breast cancer were interviewed. All participants experienced physical pain which impacted on their lives. Some were shown to have experienced deep psychological suffering which stemmed from symptoms such as odour, bleeding, festering, loss of sexual intimacy and loss of control.

I remember I did a night shift a couple of months ago and we had this woman with the most dreadful wound. I mean it was just horrible. She had a cancer of the vagina and it was fungating. She was perfectly peaceful except when we had to turn her. And we had to turn her. You have to. You can’t just leave people. If somebody needs cleaning up, you’ve got to clean them up. She didn’t have enough sedation. We gave the maximum that the doctors would prescribe. She died fairly soon after, but she was in agony while we were turning her.
Palliative care nurse
In a study of 12 women undergoing treatment in Denmark for progressive breast cancer, just under half reported that their wounds had a negative effect on their femininity. Participants in another study described their fungating wound as symbolising the end of their life, as many of the elements of their former daily life were replaced by loss of independence, embarrassment, anger, depression and fear. The odour and appearance of the wound affected the person’s romantic relationships, with the wound acting as a constant reminder to the patient and their spouse of the rapidly progressing terminal illness. One participant stated: ‘I don’t want to die, but this wound looks as if death is more and more near me. I can’t escape.’ The study concluded that while malignant fungating wounds occur infrequently, they are typically described as devastating and overwhelming.

I have seen people with open wounds. People with breast cancer where the tumour is eating through the chest wall. They are prisoners in a hospice or a hospital ward.
Palliative care consultant
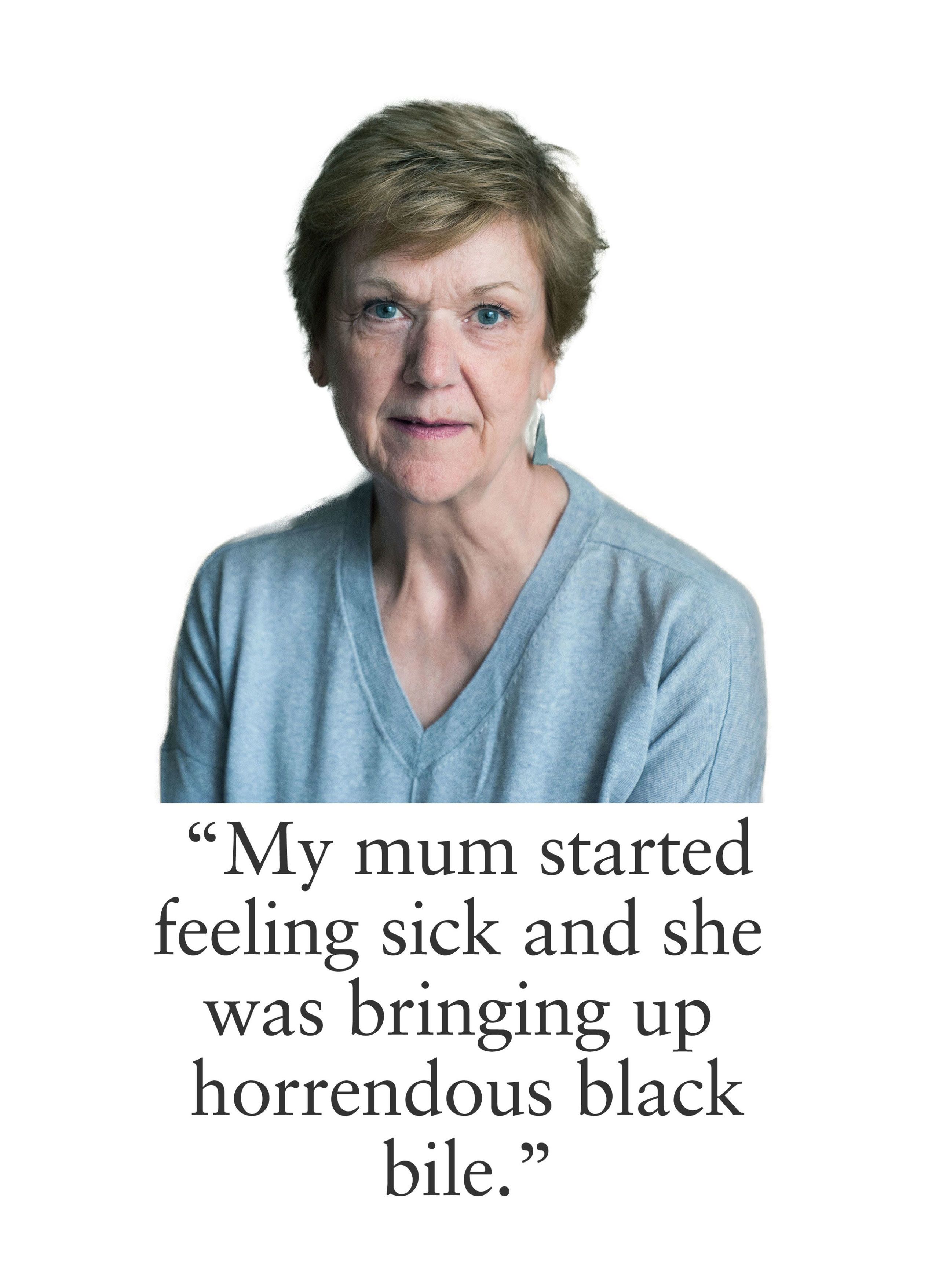
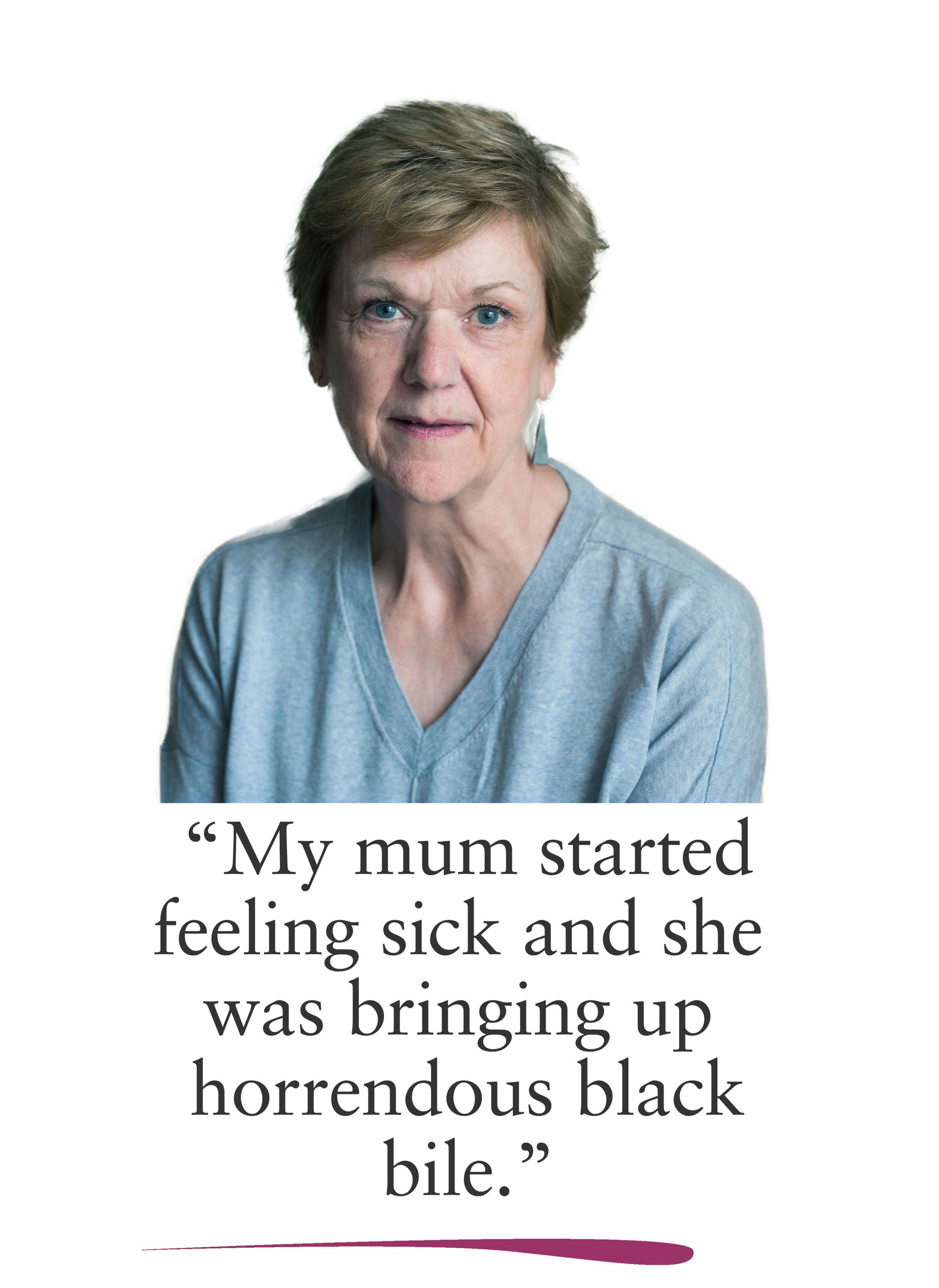
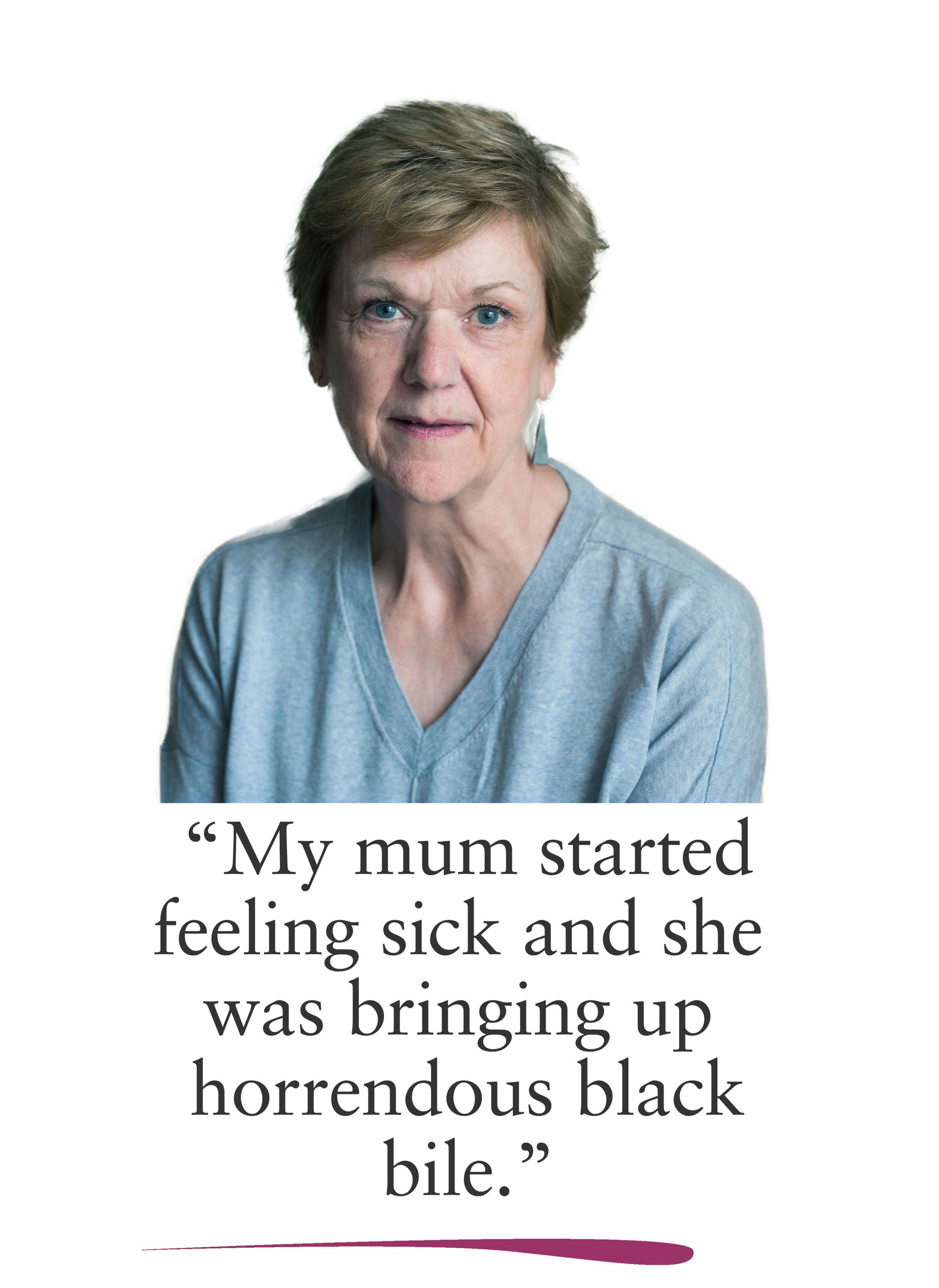
Personal story
Emma
Emma shared her experience of witnessing the death of her mother.

My mum had a lot of health issues all her life. I’m 30 now. When I was about seven she was diagnosed with a rare blood disorder. It was something like only two in one million people get it. They said most people with her condition usually live about 25 years after diagnosis. So we always knew that her lifespan would be limited.
In around 2011 she went into hospital. She’d had a blood clot in her liver and she had an associated liver disorder. You have an increased risk of getting it when you have a blood disorder. She was in a specialist unit in Leeds where they fitted a shunt in her liver and then thereafter they provided her with a fortnightly infusion of ecluzimad, a drug which helped manage her condition much better. It meant she had a better quality of life and that all went quite well for probably about four years.
Then she developed myelodysplasia, basically a leukaemia. As a result of that she started chemotherapy which then meant she had no immune system whatsoever. She did not go out because she did not want to contract infection. She didn’t see people. But obviously there is only so much you can wrap yourself up in a bubble and protect yourself from germs, so she did get an infection.
She went into hospital and we found out she had what they call necrotising fasciitis. It’s bacteria that eats your skin, eats away at your fat. If you’ve got it in a foot or an arm or something they can just amputate. But she had it in her bum and her middle area and there was nothing they could do. That was when we knew that she was terminally ill.
She had probably been in hospital a few days and I’d been to visit her. Then on the Friday I got a phone call from the doctor telling me to come in, so I knew it wasn’t good. They said she had 24 hours to live. She didn’t. She lived for 11 days.
After a few days the palliative care team came around and they were really good. They would come around daily. She had her own room which was nice, we had some element of privacy.
She was put on diamorphine and first of all it was injections as needed and then she eventually went on to a syringe driver. But we didn’t know that there were side-effects to the drugs. So at times she got anxious, distressed and confused. I was in hospital with her. I was there 24/7 and she would wake up at 3 o’clock in the morning and think there was a white rabbit in the corner of the room. All I could do was reassure her, get rid of the rabbit or whatever... For me, for both of us, that was quite frightening.
She was in a huge amount of pain because she had flesh-eating bacteria eating away at her skin. When she first went into hospital she used a bed pan and I could help her with that. But as things deteriorated she just had pads and she needed turning so they could change the pads. Some of the nurses insisted on cleaning her quite thoroughly.
She would groan in pain and I would just say to them, ‘You don’t need to do that.’ And they said, ‘Well we have to clean her thoroughly.’ ‘No, you don’t. She’s been given 24 hours to live, I don’t think she really cares. Anything that is minimally invasive and pain-free is better.’ So I always helped with that and I basically tried to instruct the carers and the nursing staff. A lot of them were good and we did it together.
Mum said to them one day, ‘Why is it going on so long? I’m still in pain.’ They gave her an increased dose and I went down to meet a friend in the canteen for a cup of coffee. When I came back she was asleep, essentially she was sedated. I’d just been out for a coffee and I didn’t know that was going to happen.
She wasn’t having such a high amount in her syringe driver. It was additional top-ups that put her to sleep. So she did open her eyes but she was under so much pain relief that that was the only movement she had, her eyes. She couldn’t do anything else. I just saw fear in her eyes and I pressed the buzzer and asked for more because I knew she was in pain.
She wanted it to be over and I didn’t want her to be there not being able to move and still in pain. From that point she was essentially sedated because I just continued to ask for more pain relief and they complied.
I was there for 11 days, so I saw everything. At the very end she was sedated. But before that she wasn’t comfortable. She was in agony. She was afraid. She was in pain for most of the time.

CURRENT PRACTICE


HASTENING DEATH
It is common for people approaching the end of life to want to hasten their deaths. A comprehensive systematic review published in 2012 found that the wish to hasten death in people with an incurable illness was associated with physical, psychological or spiritual suffering, loss of self, fear or a desire to live but ‘not in this way.’ It also reflects the search for a means to end suffering and exercise control over life.
Suicides by terminally ill people
A 2014 Freedom of Information request to Directors of Public Health found that approximately 7% of deaths recorded as suicides in England involve people who are terminally ill. This equates to over 300 dying people ending their lives every year. The World Health Organisation estimates that for each adult who dies from suicide there may be up to 20 others attempting suicide.
Bereaved relatives shared the different ways in which their loved ones had considered ending their lives.
He didn’t talk about ending it until he got to about March 2016. He let me know on the iPad, ‘I’ve had enough. I’ve had enough. I want to go.’ So I said, ‘you realise if you want to do this you’ve got to do this through Dignitas, you’ve got to do it yourself, because otherwise I could go to jail for 14 years.’
He started looking into it and I don’t know how far he actually got but he realised he’d left it too late. He didn’t actually want to do it himself. I know that because he had a very severe nut allergy which would result in full anaphylaxis. He had one or two close points over the years. I’d never had nuts in the house because it just wasn’t safe.
But from March there was a jar of nuts in the house. He could have got to it. He could have killed himself by ingesting nuts but he didn’t do it. It’s not a nice death from anaphylaxis but it’s an awful lot quicker than motor neurone disease. What he wanted was for somebody to help him – peacefully.
Healthcare professionals reported their own experiences of dying people attempting to end their lives.

A palliative care consultant I know said that she became a supporter of assisted dying when one of her patients was trying to kill himself by jumping out of a window because he was in so much distress.
GP
Research suggests the desire to hasten death is complex and informed by a number of different factors. A range of studies have found that dying people who report having a wish to hasten death do not see death as an aim in itself, but as a side-effect of pursuing the only available option of escaping suffering. While the literature is clear that many people at the end of life do experience a wish to hasten death, there is no recognised response to these wishes that can be considered universally effective.

A wish for hastened death is treated using the existing tools available to specialist palliative care teams, such as effective symptom management, talking therapies and spiritual care. However, research has shown that even when these forms of care and support are present a wish to hasten death can persist. For example, a survey of UK doctors found that in 9.8% of deaths studied, respondents reported that their patient had expressed a wish for their life to end. For 74% of these patients the wish was not shown to diminish over time. In another study, 67% of UK palliative care units surveyed reported one or more suicide attempts by patients within their care.
In 2018, Bobbie Farsides, a professor of clinical and biomedical ethics told the BMJ that she challenges 'the belief that a wish to die at a particular time and in a particular way can be “cared away,” however great the skill of the professionals and resources committed to end-of-life care.'
Stopping eating and drinking
Some people at the end of life choose to hasten their death by voluntarily stopping eating and drinking (VSED). A death by VSED means the person has actively made the decision to refuse food and water, as opposed to somebody who has lost the ability to consume food and water as a consequence of their illness.
Studies exploring deaths from VSED suggest a range of experiences. Some deaths are reported to be peaceful, with little physical suffering. Others feature pain, fatigue and impaired cognitive functioning. People initiating VSED require the support of healthcare professionals to help manage these symptoms.
While there is legal clarity that people do have the right to refuse food and water even if it brings about their death, there remains an ethical debate about VSED. In response to the death of Jean Davis, who refused food and water because she feared a drug overdose ‘would not work’, Dr Peter Saunders, former Chief Executive of the Christian Medical Fellowship, said, ‘It is not illegal to starve and dehydrate oneself to death but neither is it right.’
Some claim stopping eating and drinking is a form of suicide and believe a healthcare professional who provides medical support to someone to do it is in fact assisting them in that act.
This view suggests that it is inconsistent for legislators and medical professionals to consider VSED a legitimate end-of-life practice while simultaneously opposing legalised assisted dying.
Others argue VSED is a passive form of hastening death distinct from assisted dying and more akin to stopping life-sustaining treatment. This perspective has been used to justify the view that, while VSED could be considered a form of suicide, it is acceptable for healthcare professionals to provide palliative care to make the person’s death more comfortable.
There has been no research looking into the prevalence of VSED in the UK. Unlike other end-of-life practices, there are also no standardised guidelines in the UK for how healthcare professionals should support people who decide to hasten their death via VSED.
Regardless of the ethical debate surrounding the issue, VSED has been called ‘an imperfect but useful last resort’ when suffering persists despite the best efforts of palliative care and is known to be practised as an alternative to assisted dying.

I think in the 21st century, why are we subjecting someone to such a degrading way of dying?
Palliative care consultant
None of the healthcare professionals interviewed considered stopping eating and drinking to be a satisfactory option for dying people.





WITHDRAWING TREATMENT
Adults who have mental capacity have the right to make decisions about their own treatment and care. People can decide to consent to or refuse treatment, even if doing so may shorten their life. People choose to refuse medical treatment towards the end of their life for a range of reasons. For example, to spend more time with loved ones at home rather than be in hospital, to avoid the side-effects of treatment in order to maximise quality of life, or to avoid having life artificially prolonged.
An example of how dying people can refuse treatment with the intention to bring about their death is associated with motor neurone disease (MND). People with MND can ask doctors to remove the artificial ventilation that is keeping them alive. This requires the support of healthcare professionals, who can provide sedation when the ventilation is removed to alleviate symptoms of suffocation.
Some dying people would prefer to be able to exercise control through the option of an assisted death rather than by refusing treatment. Noel Conway, a man dying of MND, has said that he would want the option of an assisted death because if he refuses his ventilation the sedatives that will be administered ‘will cause a state of drowsy semi-consciousness until death occurs. This experience may last for a few hours or a few days; no one knows and no one can say how much that will alleviate the sensation of fighting for breath.’
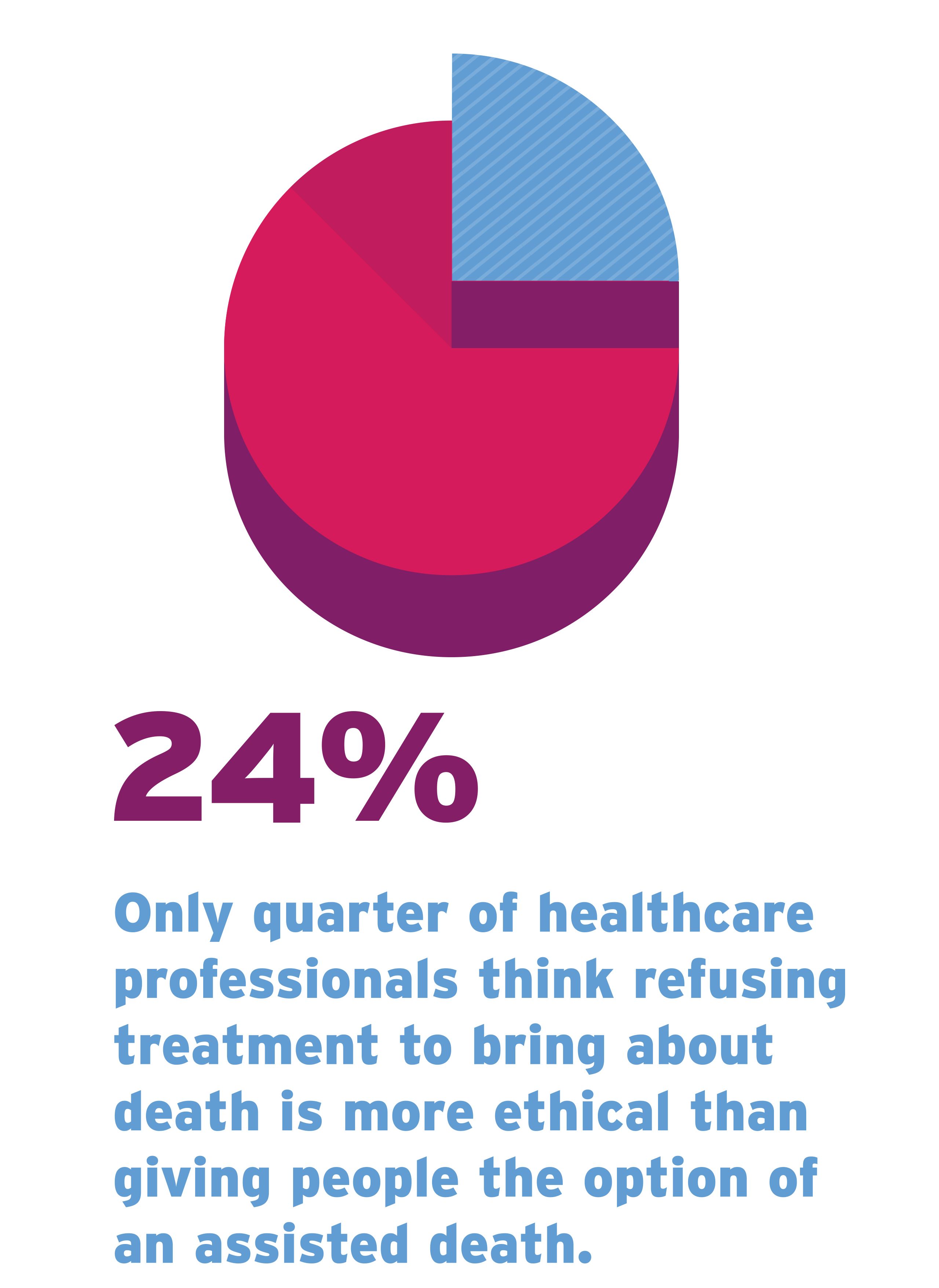
Representatives of the Association for Palliative Medicine have offered a different view. They wrote in The Times in response to Noel Conway’s legal challenge to the current law that ‘Mr Conway can die whenever he wishes. He is free to ask his doctors to remove the treatment that is artificially keeping him alive. If he does that, his doctors have a duty of care, using our specialist guidelines, to ensure that he dies peacefully.’

There’s a very thin dividing line between removing treatment and assisted dying. The intention is the same. You’re responding to a request of somebody who’s asked for it. The fact it’s possible to do that says to me, ‘Why don’t we just have assisted dying?’
Palliative care nurse
For many terminal illnesses there is no treatment that people could refuse that would enable them to hasten their death. So, whilst someone with an advanced neurological condition who is dependent on ventilation can refuse the ventilation in the knowledge they will then die, a person with terminal cancer would most probably not have a comparable option.
When a person with MND asks for their ventilation to be removed, the Association for Palliative Medicine’s specialist guidance states it is the responsibility of doctors to validate the person’s decision by ensuring that it is the ‘settled view of the patient,’ ‘that there is no coercion’ and that the patient has capacity to make the decision.
However, the inability of doctors to satisfactorily detect and address the possibility of coercion is an argument put forward by some people who oppose a change in the law on assisted dying. For example, in 2015, Dr Kathryn Mannix, a palliative care consultant, wrote in The Guardian that doctors see ‘occasional loveless families where coercion to “die sooner” would certainly occur should the law allow it.’
A few days later, in a debate in the House of Commons, Fiona Bruce MP said that proposed assisted dying legislation did not address how doctors should be satisfied that the person seeking to end their life had a ‘settled and voluntary intent’ or that there was ‘no coercion behind’ a request for an assisted death. Baroness Ilora Finlay, a former President of the Association for Palliative Medicine, has also questioned how coercion, ‘real or perceived’, can be detected.
These arguments ignore the possibility that coercion could influence end-of-life decision making under the current law and that doctors have both a responsibility and the guidance to support them to identify it. This is why the Association for Palliative Medicine refers to coercion in its literature around the removal of life-sustaining ventilation.
Safeguards in the Association for Palliative Medicine's guidance are similar to the safeguards that have been proposed in assisted dying legislation in the UK. They are also similar to the safeguards that exist in assisted dying legislation around the world.
PALLIATIVE SEDATION
Palliative sedation, also known as terminal sedation, therapeutic sedation or continuous deep sedation, is a legal end-of-life practice. Sedatives are used to relieve symptoms of suffering. Sometimes this results in the person becoming temporarily unconscious. At the very end of life somebody may be sedated and never regain consciousness.
The European Association for Palliative Care has published a framework for the use of sedation in palliative care. The framework states that sedation can be used to ‘relieve the burden of otherwise intractable suffering.’
The European Association for Palliative Care framework notes that there is no consensus within palliative care as to the appropriateness of sedation to relieve people from non-physical symptoms such as depression, anxiety or existential distress. There is also a debate around the ethical justification and clinical effectiveness of using sedation to relieve distressing symptoms experienced by people who have chosen to hasten their death by voluntarily stopping eating and drinking. The European Association for Palliative Care framework recognises that palliative sedation can be ‘profoundly distressing to family members’ as they are no longer able to interact with their loved one and the opportunity to say goodbye may be of critical importance.
Palliative sedation is an integral part of good end-of-life care. It can be effective at relieving different forms of suffering and provides many people with relief of their symptoms and a peaceful death.
As with all end-of-life practices, it is vital that there is clear communication around the use of palliative sedation and its consequences, not only between dying people and their care team but also with families, friends and carers.
In addition, evidence suggests there are circumstances where some palliative care professionals may be reluctant to instigate or use effective dosages of sedation for fear of being perceived to be hastening a person’s death. It is crucial that education and training focusses on the effective use of palliative sedation so as not to risk dying people and their families suffering unnecessarily.
Paul Chamberlain was diagnosed with motor neurone disease in 2010. In the final years of his life Paul campaigned for assisted dying because he believed the options available to him were not acceptable. Paul knew that he could ask for his artificial ventilation to be withdrawn and that his care team would administer palliative sedation to minimise any distressing symptoms. Paul died in a hospice in September 2014.
While he was denied the assisted death he campaigned for, his family described his death as peaceful and it was made possible by the use of palliative sedation. His son, Andrew, described his dad as ‘one of the lucky ones.’ Stories such as Paul’s illustrate the value of palliative sedation but existing evidence and findings from interviews with healthcare professionals, bereaved relatives and dying people show that the practice has its limitations.
Some dying people may wake unexpectedly from sedation; some may appear to be experiencing pain while not having mobility; some deaths that involve sedation can be prolonged and traumatic; in some cases, even large doses of sedatives do not achieve the intended state of unconsciousness. These cases highlight the need for other options at the end of life, including the option of assisted dying, to ensure that people do not suffer unnecessarily.
Studies have shown a disconnect between the views of dying people and healthcare professionals in regard to palliative sedation.
Many interviewees, including dying people and healthcare professionals, were unclear as to where the line between palliative sedation and assisted dying or euthanasia is drawn if the sedation results in someone being unconscious up until they die.
However, the concerns of bereaved relatives were more likely to focus on the failure of sedation in giving their loved one a peaceful death and the distress this caused. In a number of cases the use of sedation denied dying people and their family members a clear moment in which to say goodbye to one another and often resulted in a protracted death over a number of days.
It took 22 days for her to die. 11 days pretty much compos mentis and then 11 days where they stepped up the medication and she was with it but not with it, in the worst of both worlds.
Research has highlighted variations in the practice of palliative sedation, including in the role the dying person plays in the decision-making process. One recent study investigating the use of palliative sedation in European countries identified a spectrum of practice. At one end (mostly in the UK), doctors discuss the possible use of sedation with the patient, but the doctor makes the final decision over whether or not to use it. At the other end (mostly in Belgium and the Netherlands), the patient initiates the conversation and the doctor’s role is limited to evaluating whether or not appropriate criteria have been met.
In the interviews featured in this report, healthcare professionals had differing views on palliative sedation. One palliative care nurse said some of their colleagues are opposed to the practice.

Where I work there are some who are very much against palliative sedation. But, if somebody says, and they quite often do, ‘If it gets too uncomfortable and too horrible, I just want to be asleep all the time’, I would say the vast majority of nurses would be very happy with that, and I think in practice a lot of what we do does basically sedate people.
Palliative care nurse
One palliative care consultant was keen to stress that sedation is not always used to deliberately make someone unconscious. Rather, the minimum dose necessary to relieve symptoms is administered and the person may or may not become unconscious as a result of this.

We wouldn’t jump straight to sedating someone and we wouldn’t aim to sedate someone to unconsciousness, unless that is the only way in which we could treat their symptoms. But of course the side-effect of the medication is that the person might be drowsier or they might be sleepier, and so they might be less conscious as a result. I am very clear that I am not going to be aiming to make someone unconscious, but that is something that might happen.
Palliative care consultant
There is no official data on how often palliative sedation is used in the UK. In one study, 8,857 randomly sampled doctors were asked about the last death they attended. Palliative sedation was used in 17% of the deaths. In another study, 18.7% of doctors surveyed reported the use of continuous deep sedation, that is sedating someone up until the point of death, in the last death they attended. In 12.8% of the reported cases the request came from the dying person. Doctors who supported a change in the law on assisted dying, as well as doctors who did not have religious beliefs, were more likely to report using palliative sedation.
DOUBLE EFFECT
Some doctors believe there is a significant difference between administering medication with the intention of relieving suffering, even if it results in the person dying, and administering medication with the intent to end the person’s life. If the administration of medication results in the person’s death but the intention was to relieve their symptoms of suffering, then this is viewed as permissible. It is known as the principle or doctrine of double effect.
According to the British Medical Association, the doctrine of double effect has been used to differentiate, legally and ethically, between the legitimate and illegitimate use of strong opioids or sedatives at the end of life.
Double effect is a contested aspect of end-of-life care. Baroness Ilora Finlay claims ‘there is a world of difference’ between modern analgesia and assisted dying or euthanasia. In 2011, a number of palliative care consultants claimed in the BMJ that ‘there are no circumstances in which the prescription of a lethal dose of opioid is necessary to control suffering.’

I’ve got one patient at the moment. She is dying. She asked me very specifically yesterday if we could do anything to speed up her death, and if she could be drowsier. Of course we can’t do anything to speed up someone’s death, but we will do everything we can to make them comfortable and it may be that that will lead to more drowsiness. I don’t think the line is that fine. I am not saying that the medications we use are inherently, completely safe. I am just saying that the way in which they are used and increased when someone has a very limited prognosis isn’t very likely at all to hasten their death unintentionally.
Palliative care consultant
The Association for Palliative Medicine states that ‘patients may experience distress when symptoms cannot be controlled even after exhaustive attempts with specific interventions. In these circumstances some patients may require sedating medication to diminish awareness of their suffering. Medication used in this way does not shorten life.’ These claims are backed up by a number of small-scale studies which have observed that palliative sedation does not shorten the lives of people in hospice settings.
There is no consensus on the true consequences of sedatives. In 2018, one medical ethicist wrote that ‘it is at least biologically plausible that – despite their careful titration – [opioids and sedatives] do in fact hasten or bring about death.’ Therefore, the author concluded, we should be ‘agnostic’ on whether or not the use of these drugs can shorten people’s lives. Others have taken a stronger view, declaring the principle of double effect to be ‘a piece of complete sophistry.’
The European Association for Palliative Care offers a multi-faceted view. Its framework on palliative sedation describes the risk of hastened death as a possible complication of palliative sedation and acknowledges that ‘some physicians administer doses of medication, ostensibly to relieve symptoms, but with a covert intention to hasten death.’
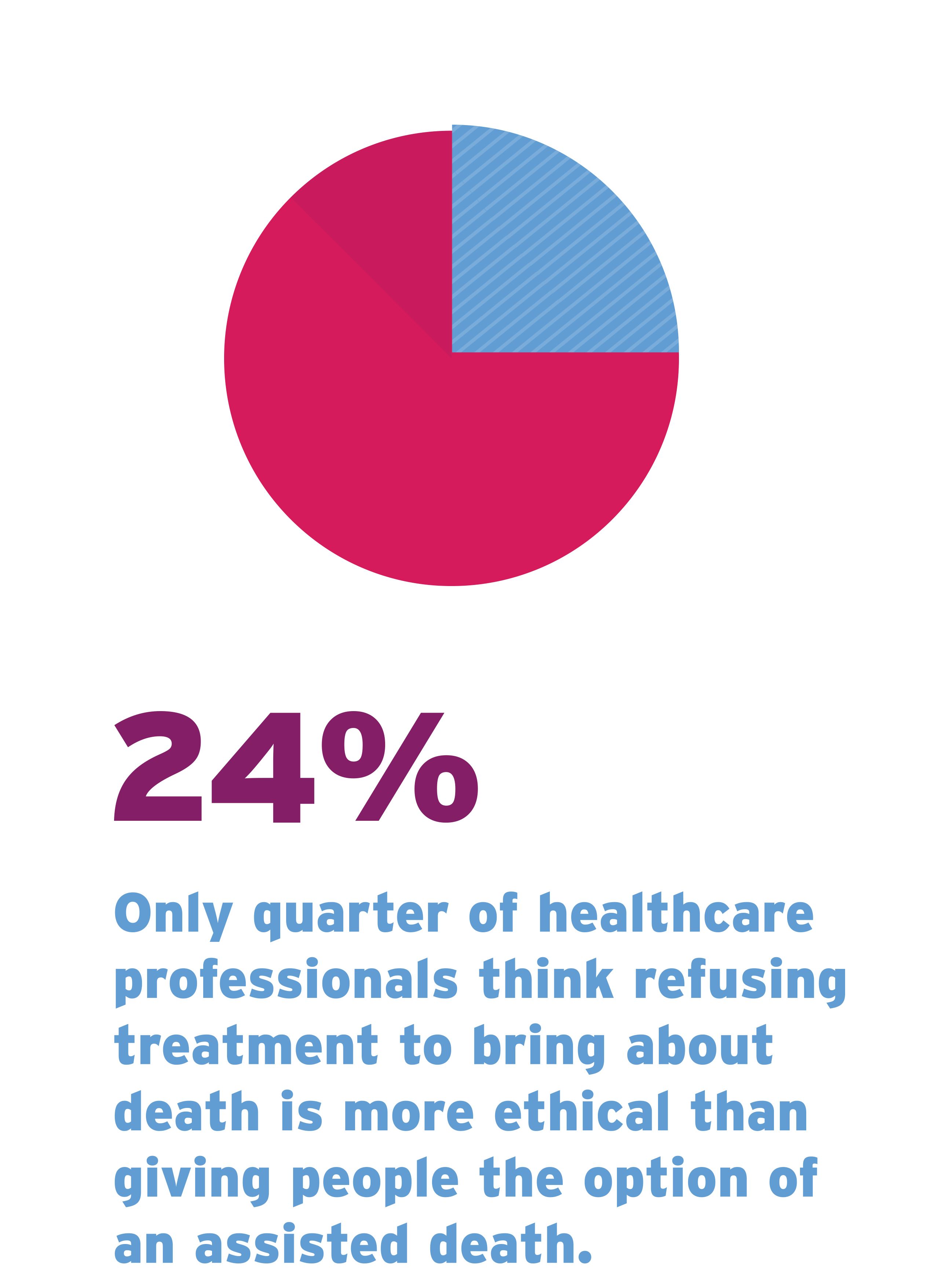
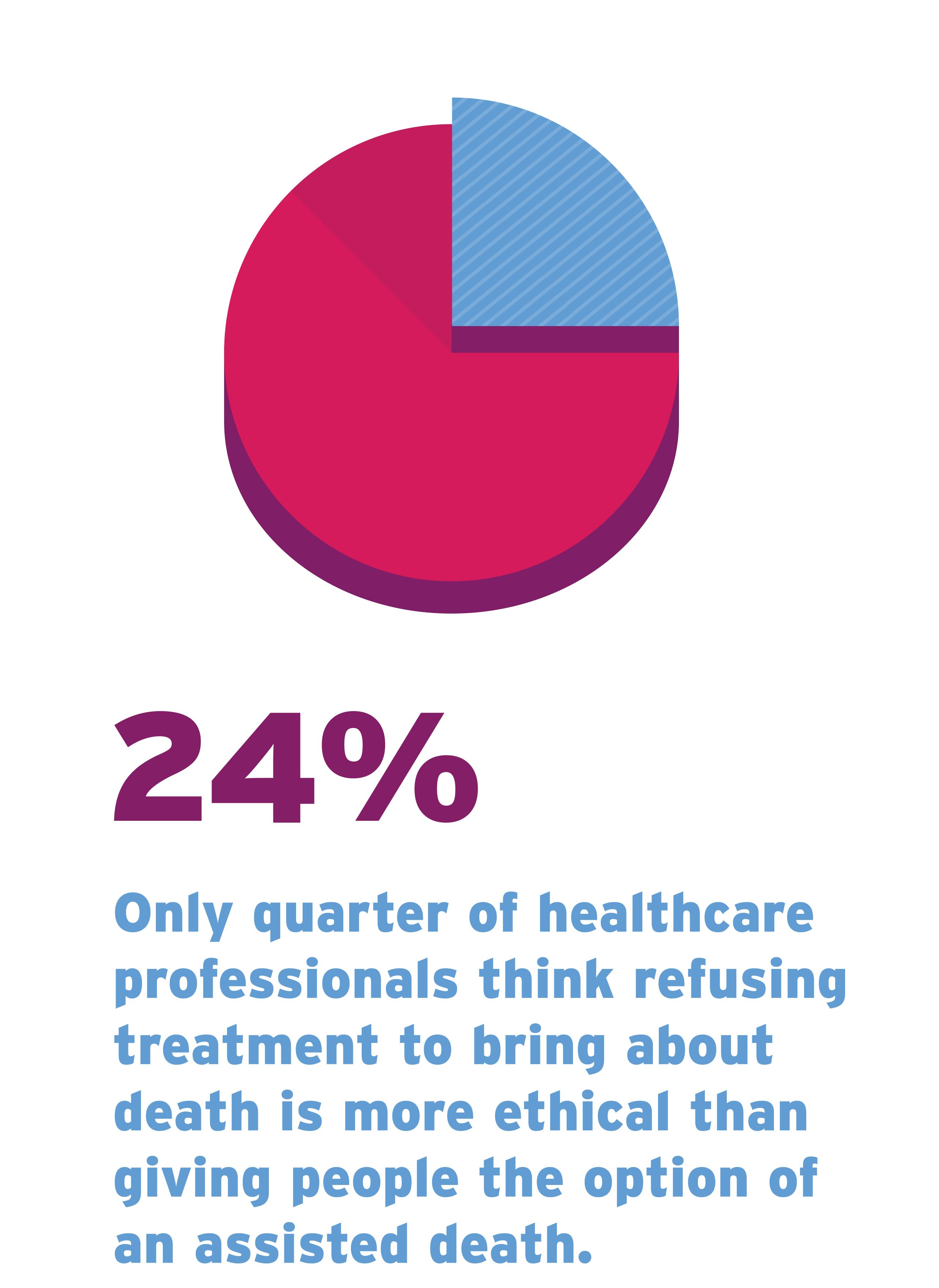
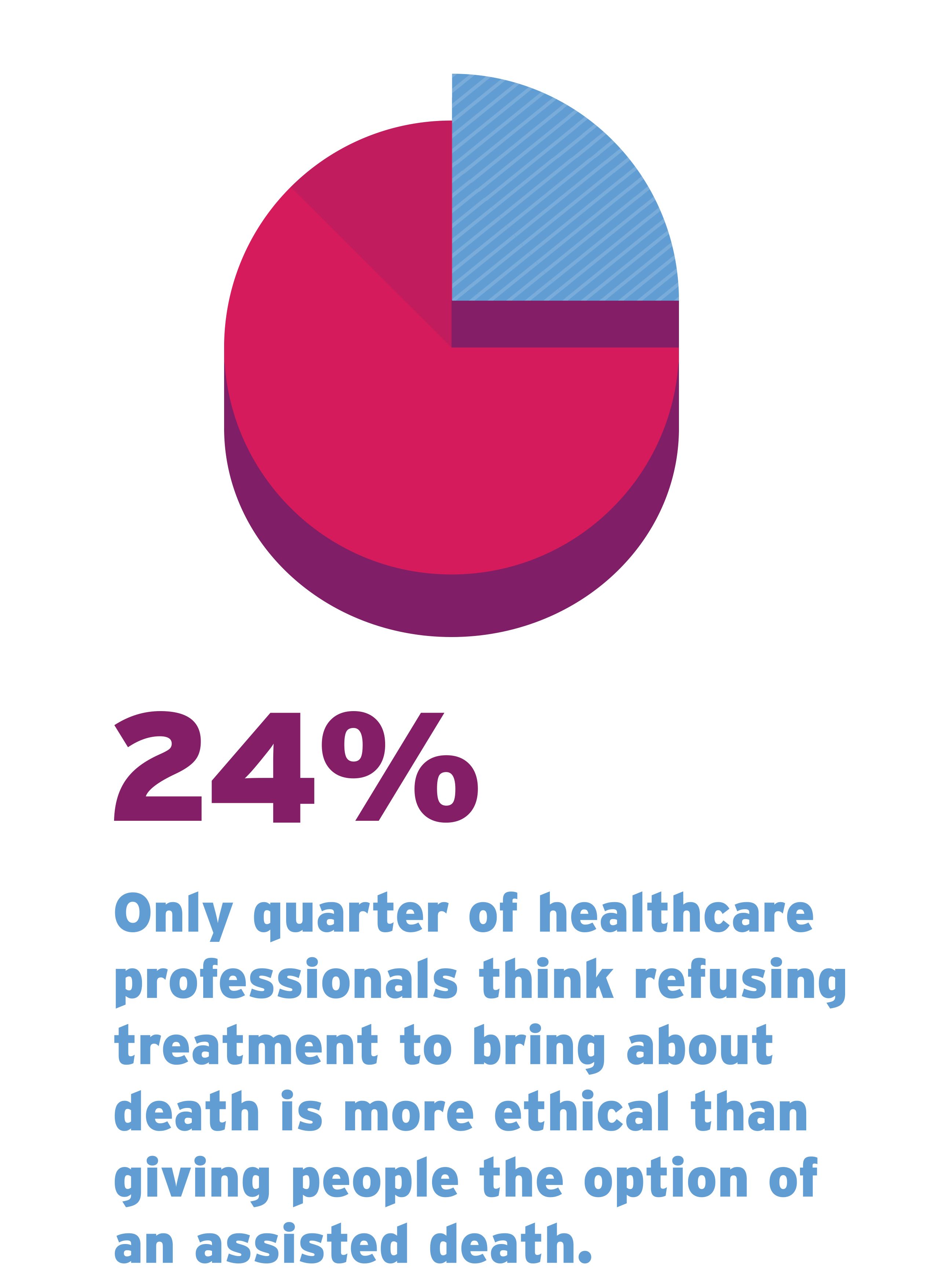
62% of healthcare professionals believe there are circumstances in the UK in which doctors or nurses have intentionally hastened death as a compassionate response to a patient’s request to end their suffering at the end of life.
A 2009 survey of doctors found that 28.9% had made decisions involving providing, withdrawing or withholding treatment that they expected would hasten the death of a person under their care. A further 7.4% reported they had made decisions with, to some degree, the intention to hasten a person’s death. These decisions were more likely to be made when responding to a person’s request for a hastened death. Some healthcare professionals discussed the possibility that former colleagues may have actively hastened death.

I think in the old days the GP came in and just did it, and I think mostly for very good reasons, and I think people were very grateful for it.
Palliative care nurse
One doctor described a patient who had asked them to end their life.

I have been asked to see people out. On one occasion a woman with carcinomas of the ovary had awful ascites – fluid in the abdomen – and her abdomen had become so distended with liquid. She was in a lot of pain and she was having palliative care but it wasn’t enough. She asked me to put her out of her misery.
GP
The disagreement surrounding the doctrine of double effect was reflected in the views of interviewees. Many struggled to see clear ethical differences between some palliative care practices and assisted dying, while others did view them as distinct.

We give medicine to treat a symptom, not to hasten the death. But you don’t know, that’s completely unquantifiable. It’s definitely a grey area. It’s blurred for everybody. It’s very difficult to quantify. How do you know how much is too much?
Palliative care doctor
Personal story
Susan
Susan describes the death of her daughter Fiona, who died in a hospice when she was 31.

She had a very painful face and the doctor sent her to the dentist. She went backwards and forwards and then she was referred to hospital. She was diagnosed with a rare form of cancer. It was a childhood cancer and it was very unusual for somebody of her age to get it.
First of all they thought it was a brain tumour, but it was actually a tumour in her paranasal sinuses which are under her eye. They wanted to start the treatment the same day. She had a course of three days of chemotherapy and then it was every couple of weeks. It went on and on.
In 2017 she was actually given the all-clear. We were delighted. The tumour was in regression and things were looking up. But unfortunately after a couple of months it reared its ugly head again.
When it grew again it grew on and behind her eye. They wanted to remove her eye but they weren’t sure whether taking it out would actually make a difference. She had to make the choice. So she kept her eye and then she had more radiation to her head, which they said was very dangerous because she could lose her short term memory. Then in December 2017 they told us that there was nothing else they could do.
In early January 2018 one of the professors at the hospital said that he thought he could remove the tumour. Again it was her decision, but they thought there was a chance that if they could remove the tumour it might give her more time. She had four operations in quick succession and each time the problem got worse. They removed her eye, but the operations aggravated the tumour and it caused it to spread.
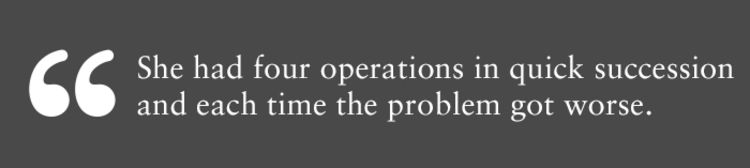
She went on a clinical trial but she was so ill. She was in hospital twice with chronic diarrhoea which burned all her bottom. All her insides were painful. She couldn’t hold her wee. She started to be in a lot of pain and in April somebody from the local hospice came to see Fiona and he said he could offer her a place in a hospice to try and manage her pain.

Prior to her going into the hospice we decided that we were going to pay for immunotherapy ourselves. The consultant at the hospital agreed it was the only course of action that could stop the progression of the disease, so we were in liaison with a professor in Harley Street. When she said to the hospice consultant that she was in a lot of pain and the consultant said, ‘What we can do is we can put you to sleep and then we can wake you up when it’s time for you to start your treatment,’ I thought that was quite weird.
In the hospice there were 11 individual rooms with a toilet for visitors and two bathrooms. I said, ‘Oh it’s strange there’s only two bathrooms for all the patients.’ I didn’t realise that all the patients there were comatose. You didn’t actually see anybody. Everybody was in bed and the only thing you heard was – it sounds awful – people screaming. In the middle of the night I used to hear people coming to take the bodies away. One weekend there were seven dead in there. It was pretty horrendous but the nurses they were all lovely. They were so nice, so helpful. Fiona was in the dayroom, she was outside in the garden, she had lots of visitors. They made it as jolly as possible.
When we were in the hospice I spoke to the consultant and she said to me that Fiona was very, very ill and in her opinion she only had days left to live. The cancer had spread and the tumour was progressing rapidly. The immunotherapy treatment was starting on 27th April, but on 26th we spoke to the professor and the consultant and in both of their opinions it wasn’t worth going ahead.
At that point Fiona had been in the hospice nearly three weeks and she was losing all mobility. It got to the stage where she couldn’t even lift her hand up and the tumour was starting to actually grow through her nose. She was having trouble breathing. We had a lot of laughs. Her humour and her joy of life – it never, ever diminished. She was in the hospice making funny videos to send to her friends and things. There was never any feeling sorry for herself.
But when we found out on 26th that the treatment wasn’t going ahead she said to me, ‘Mum, I just want them to put me to sleep. I can’t do this anymore.’
It was my son’s birthday so we decided that we were going to go ahead with the party as usual and have all the friends round and everything. On 27th the nurses came and gave her sedation and they said, ‘What will happen is you’ll be sedated and within four hours you’ll be asleep and you won’t wake up again.’ That’s what was offered and that’s what she wanted to do. I found it strange because I knew there were guidelines that they had stuck to when Fiona was in pain.

There was only a certain amount of pain relief that they were allowed to give her. She was experiencing waves of pain, breakthrough pain, and she was given top-ups. I worked out how many top-ups she had and how much they were allowed to give her the next day.
Having the sedation was her decision. It wasn’t my decision. I would have hung onto her. The nurse said, ‘I will ask you three times if that’s what you want to do.’ Fiona said, ‘No, you know I’ve thought about it.’ She wasn’t able to move. She was finding it difficult to swallow, her tongue was swollen and she was finding it difficult to talk. The tumour was growing and she was getting clots at the back of her throat. It was just awful. She was in so much pain and no matter how much pain relief she was getting, it would just exacerbate it. It was always there.
They told us she wouldn’t wake up, that she would slip away. My ex-husband came to the hospice and I got the consultant back to say the same thing, because I wanted somebody else to be there to hear it. Do you know what I mean?
On the Friday the consultant came in and she said what did Fiona want to do? Did she want to make a decision before Monday? She said that she wanted it that day. She didn’t want to wait for the weekend. We obviously thought that within hours Fiona would be asleep and that would be the end.
I was with her all night. I stayed with her all night. She was still awake. We sat around the bed and put music on but she didn’t sleep. She dozed on and off but she was awake more than she was asleep. You could have a conversation with her. She would say that she was thirsty or she wanted a drink.
She couldn’t get comfortable and she wanted me to keep moving the bed up and down because she couldn’t move but she just couldn’t get comfortable. So that was the Friday. Saturday she was still awake. Sunday she was awake. Sunday she was actually hungry. She wanted a milkshake and we went out to get her one. She had visitors.
Every day the dosage of ketamine was increasing. The consultant came in and said, ‘Oh Fiona, I can’t believe it. You’re getting serious doses of drugs.’
On the Sunday there was a lovely nurse and she said, ‘Shall we change the bed?’ And I said, ‘Yeah, I’ll help you.’ So we were changing Fiona’s bed and she had fallen asleep for a bit. It was very frightening because every time she did fall asleep we kept thinking, ‘That’s it.’ We had said goodbye and you get upset and then she’d suddenly wake up again, in a horrible way. This happened seven times. We were pleased to see her, but it was like being on a rollercoaster. It was very harrowing. Very harrowing. Your emotions are all over the place.
The nurses were also very, very upset. It was really hard for them. I felt really sorry for them. One of the nurses would often be in tears and she said, ‘There’s nothing else I can give her. I’m not allowed to give her any more. This is as much as I can give her. I can’t take the pain away for her.’
On the Monday they decided they were going to give her another syringe driver and move it from her arm to her leg. Then her breathing got shallow and shallower. The nurse came in to see her and said, ‘Oh her breathing is really shallow, I think her time’s nearly out.’ About 15 minutes later she died.
It was very distressing for Fiona because she had to keep saying goodbye to everybody. We had to say goodbye to her but she had to keep saying goodbye to all of us and that must have been awful for her. Absolutely dreadful. I wouldn’t wish it on my worst enemy. To see somebody suffer. It was torture. Her illness was traumatic enough and how she coped with it was amazing.
I still feel quite traumatised by her death because I just think that it could have been avoided.
I can’t see the difference between giving somebody large amounts of drugs to end their suffering over a period of time or giving them all in one go. It just doesn’t make sense, because the end result’s the same. I just feel that at the end of the day she was let down.
I went to this meeting in London about palliative care. There was a professor at some university who said, ‘What can we do to make people speak about dying, because people don’t broach the subject?’ We were going around the room with people saying what their views were and people said, ‘Oh yeah, I think that when I die I want to be in a middle of a field in a bed looking at the stars.’ And I thought that’s not really reality. I said, ‘Well, we broach it to a certain extent.’ Then I brought up the subject of assisted dying and I was shot down in flames and the professor swiftly moved on.
I feel like Fiona hasn’t got a voice anymore and I’m her voice. I’m the one who can tell her story and bring about change.


A BETTER WAY


Assisted dying is a legal end-of-life option for over 100 million people around the world, including in numerous states in the USA, in Canada and in Victoria, Australia.
I would feel so much safer and more confident if assisted dying were legal. It would be my judgement when I’ve had enough. It would be wonderful.
DYING PERSON

I think we just accept the fact as doctors, because we’ve been through it so many times, that it’s all awful. It’s going to be awful, but it doesn’t have to be. There is a better way.
GP
It would be indescribable, the relief that you would feel knowing you had access to that if need be. It would be a massive comfort.
DYING PERSON
CONCLUSION
This report exposes a truth about dying that is often ignored and sometimes even mistakenly denied: like all areas of medicine, specialist palliative care has its limits.
The more detailed version of this report is available to read below.
The nature of these limitations means that, whilst the majority of dying people will have their symptoms managed, a small but significant minority of people will suffer intolerably throughout the final months, weeks and days of their lives.
This is not an argument against specialist palliative care or an effort to diminish the valuable work of those who provide care at the end of life more broadly. On the contrary, campaigners for assisted dying recognise this vital work and support all efforts to improve the quality of care in this country through investment, research and improved access.
However, even if there was universal access to the highest quality care, some people would still have no relief of their pain as they died. This is what is happening for dying people at present. Others suffer with symptoms that they feel rob them of their dignity.
What these dying people go through, against their wishes, could be regarded as the collateral damage of maintaining the prohibition of assisted dying.
The experiences shared in this report do not represent the majority but they do reflect the reality of dying for a small but significant group, and they should not be ignored.
The prospect of experiencing such physical or emotional distress causes dying people to fear the future. This fear can be a form of suffering in itself, leading to a reduction in quality of life. In contrast, having the option of an assisted death would be a source of comfort and reassurance to many dying people.
An examination of end-of-life practices reveals the line between the current law and assisted dying is often blurred and this raises ethical questions for healthcare professionals to which there are no clear answers.
In this context, assisted dying would not be a substantial departure from what is happening now, but it would provide a safe, transparent and compassionate option for those who wish to control the manner and timing of their deaths.
HELP US END THE SUFFERING
Will you speak out for the 17 people who are suffering today?
SUPPORT
The following organisations can provide information and support to people who would like information on terminal illnesses, end-of-life care and bereavement.
- Bowel Cancer UK
020 7940 1760
www.bowelcanceruk.org.uk - Brain and Spine Foundation
0808 808 1000
www.brainandspine.org.uk - Breast Cancer Care
0808 800 6000
www.breastcancercare.org.uk - Compassion in Dying
0800 999 2434
www.compassionindying.org.uk - Cruse Bereavement Care
0808 808 1677
www.cruse.org.uk - Cruse Bereavement Care Scotland
0845 600 2227
www.crusescotland.org.uk - Hospice UK
020 7520 8200
www.hospiceuk.org - Macmillan Cancer Support
0808 808 00 00
www.macmillan.org.uk - Marie Curie
0800 090 2309
www.mariecurie.org.uk - Motor Neurone Disease Association
0808 802 6262
www.mndassociation.org - MND Scotland
0141 332 3903
www.mndscotland.org.uk - Oesophageal Patients Association
0121 704 9860
www.opa.org.uk - Ovarian Cancer Action
0300 456 4700
www.ovarian.org.uk - Samaritans
116 123
www.samaritans.org - Sue Ryder
0808 164 4572
www.sueryder.org
Have you been affected by this issue?
The people in this report decided to share their experience because they believe the law should change. We know there are many more stories like the ones outlined in this report.
If you have a story to share, particularly if you are living with a terminal illness, have witnessed a loved one suffer a bad death or have accompanied someone abroad to have an assisted death, please let us know using the form below.
Dignity in Dying campaigns for greater choice, control and access to services at the end of life. It advocates providing terminally ill adults with the option of an assisted death, within strict legal safeguards, and for universal access to high quality end-of-life care.
CREDITS
Online producer: Zach Moss
Author: Lloyd Riley and Davina Hehir
Research support: Hannah Easdown and Upeka De Silva
Research interviews: Professor Bronwyn Parry and Sally Eales
Photography: Luke Doyle
Publication date: 2 September 2019